Fatigue and sweating after COVID describe ongoing physical changes that some people notice after a SARS-CoV-2 infection. These symptoms can appear together or separately.
They may last beyond the first illness phase. They are usually linked to changes in the nervous system, immune response, and circulation, not to active infection. The course and intensity differ from person to person.
This article explains fatigue and sweating after COVID clearly and medically. It focuses on causes, timing, and when symptoms may need review.
Educational platforms such as SensIQ work to explain complex brain and body processes using evidence-based information. The sections below describe what the research suggests and what remains uncertain.
Key Takeaways
- Fatigue and sweating after COVID can persist for weeks or months due to lingering effects on the immune, nervous, and cardiovascular systems rather than active infection.
- These symptoms often fluctuate and may include dizziness, heat sensitivity, or brain fog, affecting daily energy and focus.
- Sweating without fever can result from autonomic nervous system changes, sometimes overlapping with conditions like postural orthostatic tachycardia syndrome (POTS).
- Medical evaluation is advised if fatigue or sweating interferes with everyday activities, worsens over time, or is linked to changes in heart rate or blood pressure.
Research continues to explore why some people develop long-lasting symptoms while others recover quickly, highlighting the need for individualized assessment and ongoing study.
Why does fatigue and sweating happen after COVID?
Fatigue and sweating after COVID are thought to come from the lasting effects of a SARS-CoV-2 infection. Research suggests that immune activity, nerve signals, and blood vessel control can stay altered after the acute illness¹.
These changes can affect energy, body temperature, and circulation. This may explain why symptoms continue even when tests look normal.
Autonomic nervous system changes
The autonomic nervous system controls functions you do not think about, such as heart rate, blood pressure, and sweating. In some post covid cases, this system reacts differently to movement or standing².
This can lead to fatigue and sweating post covid during light activity. Some long COVID patients also notice dizziness or a racing heart.
Inflammation and immune response
Low-level inflammation has been found in people with long COVID. Immune signals can disrupt how the body uses energy and controls heat. This can increase physical or mental fatigue and make heat harder to tolerate. Similar patterns are seen in chronic fatigue syndrome.
What fatigue and sweating after COVID feel like
Many people say this fatigue feels different from normal tiredness. It may include heavy limbs, slow thinking, or trouble focusing, sometimes called fatigue brain fog. Sweating can start suddenly and without a clear cause. Symptoms often change from day to day.
These symptoms can reduce the quality of life. Daily tasks may take more effort or require rest afterward. People with long COVID often say recovery feels slower than expected. This experience is not the same as being out of shape.
Sweating after COVID, with or without fever

Sweating after COVID does not always come with a fever. Many people report night sweats, heat sensitivity, or sweating during mild activity. Body temperature may stay normal. These symptoms often relate to nervous system control rather than infection.
Some people also notice changes in heart rate or blood pressure when they stand. This pattern can resemble postural orthostatic tachycardia syndrome POTS, which has been reported in some people with long covid³. Not everyone with sweating symptoms has this condition.
How long do fatigue and sweating post-COVID last
The length of symptoms varies. Some people improve within weeks. Others report symptoms for months or longer. Fatigue and sweating after COVID describe ongoing physical changes that some people notice after a SARS-CoV-2 infection. Recovery is often uneven.
Illness severity, past health, and stress may affect recovery time. Many people with long COVID describe good days followed by worse days. This makes it hard to predict timelines.
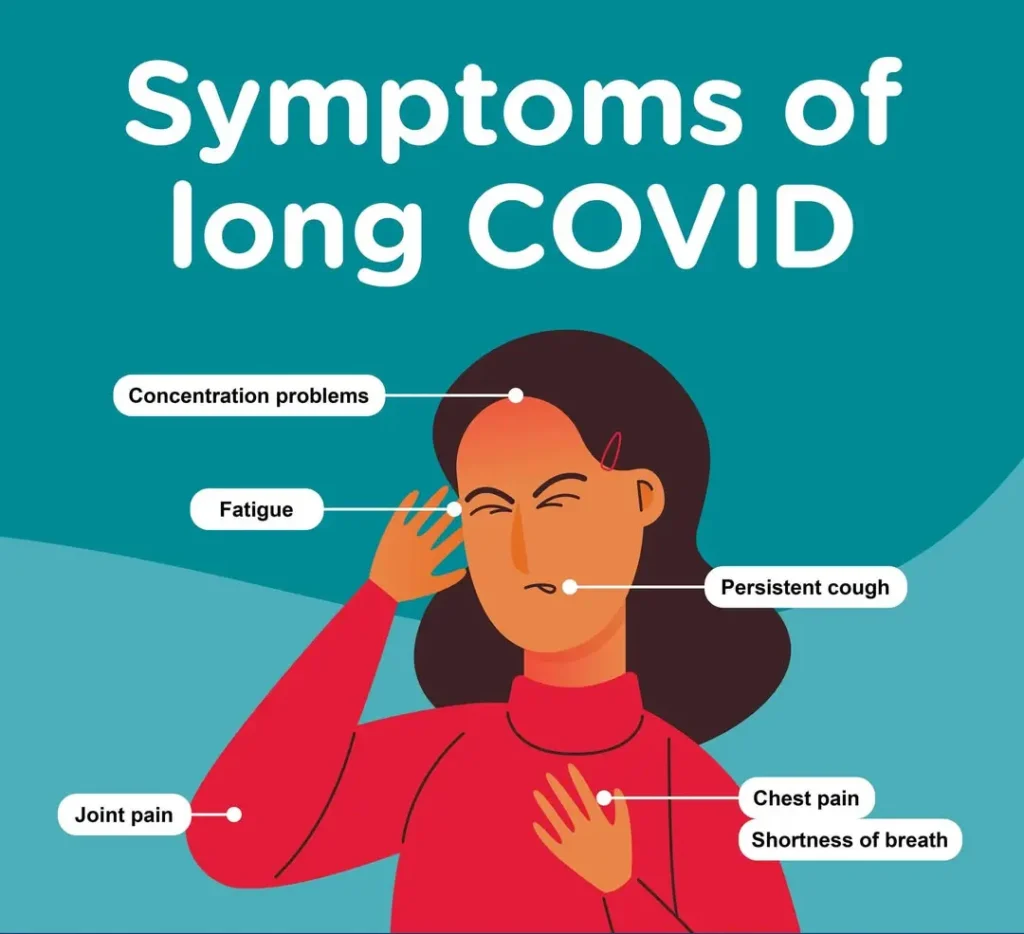
Common lingering and long COVID symptoms
Common symptoms beyond fatigue and sweating
Fatigue and sweating are common symptoms, but they are rarely the only ones. Other symptoms of long COVID include shortness of breath, sleep problems, muscle pain, and thinking changes¹. Some people also notice effects on mental health. Symptoms differ between individuals.
Long COVID patients often report persistent symptoms that affect physical or mental function. These issues can limit activity and social life. Looking at the full symptom pattern helps explain why recovery may take time.
Why symptoms may appear weeks after infection
Some post covid symptoms start weeks after the initial illness². People may feel better at first, only to develop new symptoms later. This delay may reflect slow changes in immune or nerve responses. It does not mean the virus is still active.
Post-exertional malaise PEM is one pattern seen in people with long COVID. Symptoms worsen after physical or mental effort. The effect may appear hours or days later. This differs from normal tiredness.
When fatigue and sweating after COVID need medical review
Medical review is essential when symptoms limit daily life, worsen, or cause concern. Warning signs include chest pain, fainting, or significant changes in blood pressure or heart rate. Evaluation helps rule out other causes. Ongoing symptoms should not be ignored.
Clinicians also assess how symptoms affect quality of life and daily functioning. Early review can support monitoring and guidance. Subsequent steps depend on symptom type and severity.
How clinicians assess and manage long COVID symptoms
Evaluation usually includes a detailed symptom history and physical exam. Clinicians may check heart rate, blood pressure, and response to activity. Long COVID treatment focuses on managing symptoms rather than using a single approach⁴. Care plans are adjusted over time.
Dr. Luke Barr, Chief Medical Officer at SensIQ, notes that careful assessment helps clarify symptom patterns. This supports an accurate understanding rather than broad assumptions. Medical guidance continues to change as research grows.
What research still does not fully explain
Researchers still do not know why some people develop persistent symptoms while others recover quickly. Different biological pathways may be involved. Predicting recovery time remains difficult. Studies are ongoing to understand long COVID better.
Recognizing these limits supports realistic expectations. Clear information helps people make informed choices. Continued long COVID recovery research is needed to improve care and understanding.*
References
- Centers for Disease Control and Prevention. (2025). Long COVID Signs and Symptoms. U.S. Department of Health and Human Services. https://www.cdc.gov/long-covid/signs-symptoms/index.html
- Yale Medicine. (2024). Long COVID (post-COVID conditions PCC). Yale School of Medicine. https://www.yalemedicine.org/conditions/long-covid-post-covid-conditions-pcc
- Raj SR, Arnold AC, Barboi A, Claydon VE, Limberg JK, Lucci VM, Numan M, Peltier A, Snapper H, Vernino S; American Autonomic Society (2021). Long-COVID postural tachycardia syndrome: an American Autonomic Society statement. Clin Auton Res. Jun;31(3):365-368. doi: 10.1007/s10286-021-00798-2. https://pubmed.ncbi.nlm.nih.gov/33740207/
- World Health Organization. (2020). Post COVID-19 conditions. https://www.who.int/teams/health-care-readiness/post-covid-19-condition
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.