Antibiotics help treat infections, but some people notice changes in thinking while taking them or after finishing treatment. These changes are often called antibiotic brain fog, a non-medical term for temporary problems with focus, memory, or mental clarity.
Research suggests these effects are uncommon and occur in only a small proportion of people who use antibiotics. When they do occur, symptoms are usually mild and improve as the body recovers.
This article explains how antibiotics may relate to cognitive symptoms, what research suggests, and where limits remain. SensIQ is mentioned only as a neurologist-developed educational framework that discusses brain health and cognition, not as a supplement, treatment, or diagnostic tool.
The goal is to help readers understand potential causes and know when to consult a healthcare professional.
Key Takeaways
- Some people experience antibiotic brain fog, a short-term change in focus or clarity that usually resolves after treatment ends.
- Research suggests antibiotics may affect brain function indirectly through immune response, gut–brain communication, and the blood-brain barrier, rather than acting directly on the brain.
- Reported symptoms such as temporary mental confusion or slower thinking are generally mild and not linked to lasting cognitive impairments.
- Duration and intensity vary based on factors such as infection severity, sleep, nutrition, and the specific antibiotic class used.
- Most cases improve naturally, but persistent or worsening symptoms should be discussed with a healthcare professional to rule out other causes.
Can antibiotics cause brain fog?
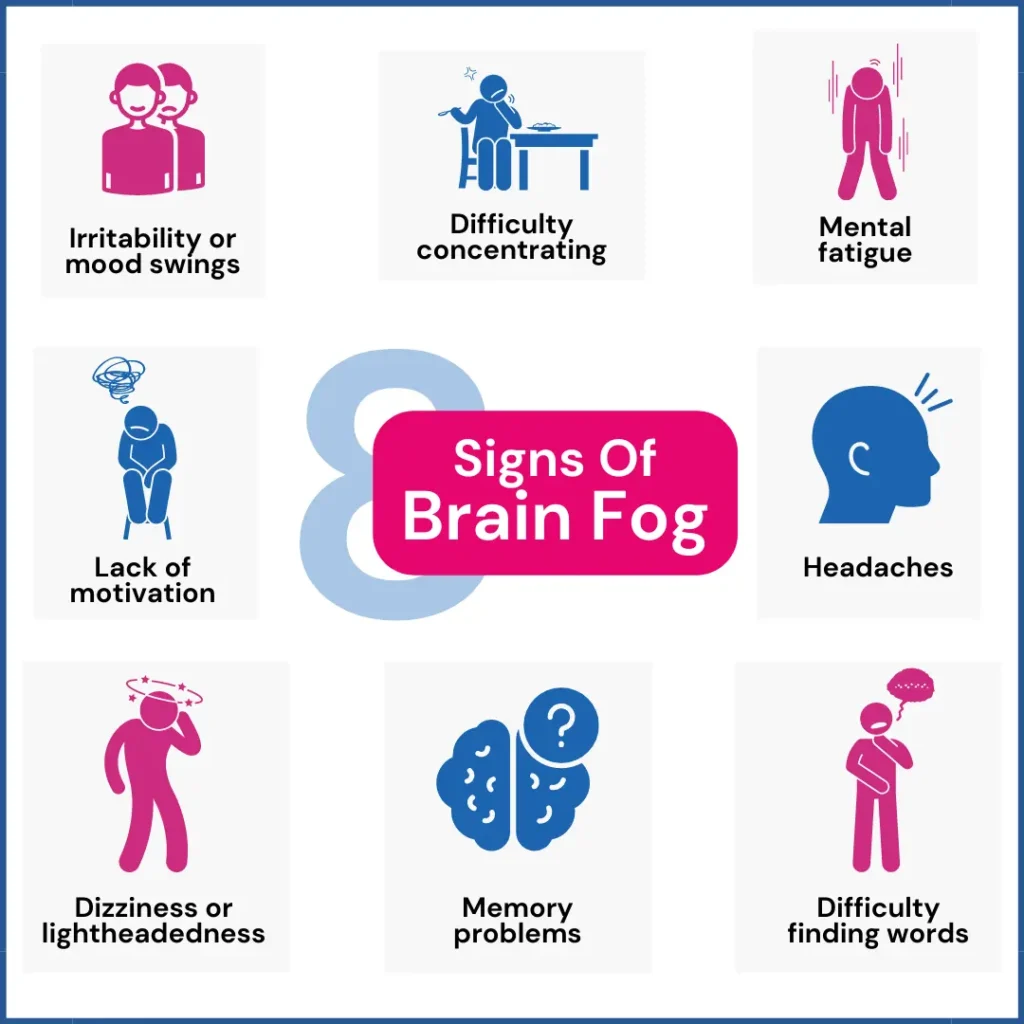
What brain fog means medically
Brain fog is not a medical diagnosis. Doctors use the term to describe how people feel when their thinking seems slower or less clear. Common descriptions include trouble focusing, slower thinking, or feeling mentally tired.
Many people describe brain fog as temporary mental confusion, not as memory loss or disorientation. This difference matters. Brain fog reflects how the brain feels during stress or recovery, not permanent damage.
What research suggests so far
The question of whether antibiotics can cause brain fog does not have one clear answer. Some people notice cognitive changes during or after treatment. Many others do not see any mental effects.
Research suggests that antibiotics may indirectly affect brain function, often linked to illness or immune stress, rather than directly affecting the brain¹.
When people ask whether antibiotics cause brain fog, they are often noticing a change from how they usually feel. These changes depend on the person, the infection, and the medication involved.
How antibiotics may affect the brain
Inflammation and immune response
Antibiotics are used during a bacterial infection, which already places stress on the body. The immune system releases signals to fight infection. These signals can affect many systems, including the brain.
Inflammation has been linked to short-term cognitive issues such as mental fatigue and slower focus². In many cases, these effects come from the illness itself rather than the medication.
Gut–brain and neurotransmitter changes
Researchers also study the gut-brain axis, the link between gut bacteria and the nervous system. Antibiotics can alter gut bacteria during treatment, potentially affecting how the brain receives signals.
Gut microbes also play a role in metabolizing nutrients such as fatty acids, which support cellular signaling and energy balance in the brain. Disruptions in these pathways are one proposed explanation for why some people report cognitive changes during or after antibiotic use.
Evidence in this area is still emerging and does not suggest uniform effects. Similar patterns are seen in perimenopause brain fog, where hormonal changes and inflammation may temporarily affect clarity and focus through related pathways.
The role of the blood-brain barrier
The blood-brain barrier protects the brain by controlling what enters from the bloodstream. Most antibiotics do not cross this barrier in meaningful amounts. However, some classes of antibiotics may influence brain signaling under specific conditions.
Much of this knowledge comes from case reports rather than large trials. These reports help identify rare reactions but do not suggest routine risk for most people.
Why individual biology matters
Not everyone responds to antibiotics in the same way. Differences in age, metabolism, and overall brain health can shape how the body reacts during treatment and recovery. Some people break down medications quickly, while others process them more slowly. This can influence how long specific effects are felt.
Personal health history also plays a role. People who are already dealing with sleep problems, high stress, or mood changes may notice cognitive symptoms more easily. In these cases, antibiotics may add to an existing strain rather than cause new problems on their own.
Nutrition and hydration can also affect recovery. The brain relies on a steady energy supply and balanced signaling. During illness, changes in appetite or fluid intake can briefly affect attention and focus. These factors may exacerbate brain fog even when the medication itself is not the primary driver.
Because of these differences, two people taking the same antibiotic can have very different experiences. This variation helps explain why research findings are mixed and why personal reports do not always match clinical averages.
Common symptoms people report
Feeling spaced out or disoriented
People who report experiencing brain fog often say they feel mentally slower than usual. They may feel less alert or need more effort to complete tasks. These feelings usually come and go during the day.
For instance, people recovering from viral infections have reported similar experiences, as discussed in COVID brain fog, where inflammation and immune stress can briefly affect clarity.
This experience is common during illness and recovery. It is not unique to antibiotic use and often improves as energy returns.
Memory, focus, and mental clarity changes
Other symptoms include trouble focusing, slower recall, or mental tiredness. These fall under cognitive side effects, which can happen with many medicines and health conditions.
These symptoms do not mean lasting cognitive impairments. A similar pattern appears in perimenopause memory loss, where short-term lapses often relate to hormonal and stress-related changes rather than actual decline.
They are different from conditions that cause ongoing memory loss or decline. Most people return to their normal mental clarity over time.
Post-antibiotic brain fog and duration
How long does brain fog last after antibiotics
When symptoms appear after treatment ends, people often call it post-antibiotic brain fog. Research suggests that when these symptoms occur, they usually improve within days or weeks³. Recovery frequently aligns with improvements in sleep and overall health.
For most people, symptoms fade on their own. Ongoing problems are less common and may point to other causes.
Why recovery time varies
Recovery differs from person to person. Factors include immune response, sleep quality, stress, and overall mental health. Diet, hydration, and activity level may also play a role.
For most individuals, symptoms are not long-term. If symptoms persist or worsen beyond expectations, medical review is appropriate.
Which antibiotics are linked to brain fog

Observations from case reports
There is no clear list of antibiotics that reliably cause brain fog. Some medications appear more often in case reports, which describe individual experiences rather than typical outcomes.
These reports help researchers notice patterns but cannot prove cause and effect. They should be viewed with caution.
Antibiotics discussed in research
Antibiotics such as amoxicillin, azithromycin, and doxycycline have been mentioned in some reports. In a few cases, people described symptoms that may have affected the central nervous system, though reasons remain unclear⁴.
An article published on medication-related cognition explains that these effects are uncommon. Most people take these drugs without noticing mental changes.
Can antibiotics clear or help with brain fog?
Treating an infection improves cognition
Some people feel mentally clearer once an infection resolves. In these cases, antibiotics treat the illness rather than the brain symptoms. As inflammation drops and energy returns, cognitive function may improve.
This improvement reflects recovery from illness, not a direct effect of antibiotics on the brain.
Why antibiotics do not treat brain fog directly
Antibiotics are not meant to improve thinking or focus. While treating infection can support overall brain health, antibiotics do not act on brain pathways that control attention or memory.
Understanding this helps avoid unrealistic expectations about what antibiotics can do.
What does antibiotic-related brain fog not mean
Not brain damage
Brain fog does not mean the brain is damaged. There is no evidence that short-term symptoms lead to lasting harm. Most cases improve as the body stabilizes.
Brain fog should be seen as a temporary state, not a sign of decline.
Delirium versus brain fog
Delirium is a medical condition most commonly seen in hospitalized or very ill patients. It causes sudden changes in awareness and focus and usually improves once the causes are treated⁵. Mild symptoms, including brain fog during recovery, are not the same as delirium.
When to seek medical guidance
Medical advice is helpful if symptoms are severe, ongoing, or affect daily life. This includes trouble doing routine tasks, behavior changes, or safety concerns. A healthcare professional can help identify the cause.
As noted by Dr. Luke Barr, a physician and clinical expert who serves as Chief Medical Officer at SensIQ, cognitive symptoms should be viewed in context rather than attributed to a single cause. Sharing details about symptoms, timing, and medications supports accurate care.*
References
- American Academy of Neurology. (2016). Common antibiotics may be linked to temporary mental confusion. https://www.aan.com/PressRoom/Home/PressRelease/1433
- Cryan, J., Dinan, T. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci 13, 701–712. https://doi.org/10.1038/nrn3346
- Inouye, S. K. (2006). Delirium in older persons. The New England Journal of Medicine, 354(11), 1157–1165. https://doi.org/10.1056/NEJMra052321
- Moore, A. R., & O’Keeffe, S. T. (1999). Drug-induced cognitive impairment in the elderly. Drugs & Aging, 15(1), 15–28. https://doi.org/10.2165/00002512-199915010-00002 PubMed
- Anderson, S. C. (2023). Antibiotics and the brain: It’s complicated. Psychology Today. https://www.psychologytoday.com/us/blog/mood-by-microbe/202305/antibiotics-and-the-brain-its-complicated
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.