Most women can consider supplements for menopause joint pain as one part of a broader, conservative plan. Hormone shifts can sensitize joints and soft tissue, so supportive nutrients, movement, and sleep strategies may help some people.
Research suggests specific options may support a healthy inflammatory response, while overall joint health improves with structured lifestyle steps and clinical oversight when needed. No single option fits everyone, and choices should reflect symptoms, risks, and preferences.
This article explains why joint pain during menopause can rise, which options might help, and how to use them safely.
SensIQ appears here as a neurologist-developed educational resource focused on clear, evidence-based guidance. You will see how mechanisms, safety, and practical steps connect, with citations for key claims and cautious language.
Key Takeaways
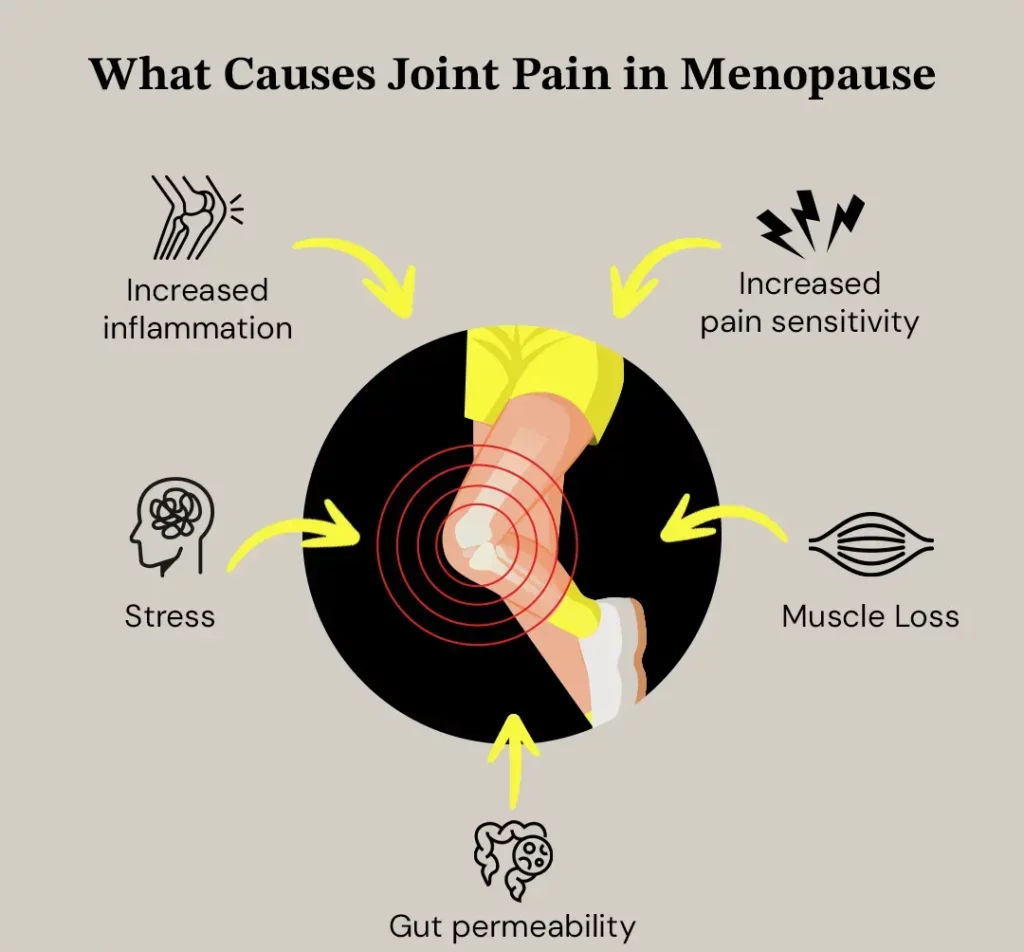
- Hormonal fluctuations during menopause can affect inflammation, pain sensitivity, and connective tissue, leading many women to experience varying levels of joint and muscle discomfort.
- Supplements for menopause joint pain may support joint health and comfort when used responsibly, but they should complement, not replace, medical evaluation or lifestyle measures.
Nutrients such as omega-3 fatty acids, curcumin, collagen, glucosamine, vitamin D, and calcium may help support a healthy inflammatory response and bone density, though results vary among individuals. - Regular exercise, weight-bearing movement, adequate sleep, and maintaining a healthy weight remain the most consistent natural remedies for long-term joint health.
- Always consult a healthcare professional before starting or changing any supplement routine to ensure safety, avoid interactions, and personalize your menopause joint pain relief plan.
Why Menopause Causes Joint Pain
Hormone levels fluctuate through perimenopause, and many women experience stiffness or joint pain during menopause as a result. Estrogen variation can influence pain signaling, connective tissue hydration, and inflammatory pathways, thereby affecting daily comfort.
Observational data suggest arthralgia is common during this transition. However, intensity and timing vary widely, with some women also reporting menopause and hip joint pain as part of the same process. Clinicians also consider age-related changes and coexisting conditions when assessing symptoms.
Hormone shifts and inflammation
Lower or variable estrogen levels can alter cytokine levels and pain perception, potentially increasing background sensitivity. Some women also report hot flashes and night sweats that disrupt sleep, which can lower pain tolerance the next day.
These patterns are real, yet not universal, and they often fluctuate month to month. Personal history, medications, and activity patterns also matter.
Which hormone helps with joint pain
Menopause societies note that hormone replacement therapy (HRT) is effective for vasomotor symptoms and may be considered for joint symptoms in select contexts, but it is not a universal solution.
Shared decision-making weighs benefits, risks, and side effects. When HRT is not suitable, nonhormonal options and supportive strategies remain available.¹
Why joint and muscle pain overlap
Tendons and muscles respond to load, sleep, and stress, which explains why women experience both joint and muscle discomfort. Many also ask, can menopause cause hip and leg pain?, since hormonal and mechanical factors often affect multiple lower-body joints at once.
Periods of inactivity or weight gain can add mechanical strain. A simple plan that restores movement and recovery frequently helps maintain quality of life.
Supplements for Menopause Joint Pain Relief
Supplements can support a broader plan when chosen carefully. The question is not which capsule relieves pain, but which nutrients align with your goals, risks, and current diet.
Discuss interactions, dosing, and monitoring, and set realistic expectations before starting. Evidence supports some ingredients as adjuncts rather than stand-alone fixes.²
Do supplements help with menopause joint pain relief?
Data are mixed, yet specific nutrients have plausible mechanisms and early evidence. Some options may help reduce inflammation as part of a healthy inflammatory response, especially when combined with exercise and sleep. Use time-boxed trials with clear stop rules, and review progress with your clinician.³
What is the best supplement for menopausal joint pain?
“Best” depends on your profile, other medications, and the symptoms you want to change. Review options with a clinician, confirm ingredient amounts and third-party testing, and understand possible side effects. Supplements do not replace medical care, and avoiding multiple new products at once helps you evaluate response.
Natural supplements for menopause joint pain
Commonly discussed options include omega-3 fatty acids, curcumin, collagen peptides, and glucosamine, as well as SensIQ’s natural health joint supplement for those exploring additional supportive formulations.
Quality varies by brand, so verify independent testing. Track sleep, activity, and comfort in a simple log to judge usefulness over four to eight weeks, and remember that results may vary.
Best supplements for menopause muscle pain
Muscle soreness may relate to overall load, protein adequacy, and vitamin D status. Combine any supplement trial with progressive strength training and mobility, rather than rest alone. Reassess if you see no change after a fair trial and adjust the plan as needed.

Important Supplements and Nutrients
Ingredient-level decisions work better when you know the expected role, the dose range, and the limits. Start low, add one change at a time, and evaluate with simple metrics that matter to you. Align choices with diet quality, training plan, and sleep.*
Omega-3 and anti-inflammatory nutrients
EPA (Eicosapentaenoic Acid) and DHA (Docosahexaenoic Acid) from fatty fish or concentrated oils may help reduce markers of inflammation in a healthy inflammatory response.
However, results vary by dose and duration. Consider dietary sources like fatty fish first, then discuss capsules if intake is low. Monitor for interactions, especially with anticoagulants, and set a specific trial window.³
Curcumin
Curcumin has been studied for supporting a healthy inflammatory response, but bioavailability differs across products. If you trial it, use standardized extracts, and watch for gastrointestinal side effects. Stop if you see no clear benefit after a set period, and record changes in function, not just soreness.
Glucosamine
Glucosamine is often discussed for cartilage support, yet its effects appear small and inconsistent. If you try it, choose one variable at a time to isolate impact. Reassess with functional measures and note that results may vary.
Collagen
Collagen peptides may support connective tissue and comfort in some populations. Pair collagen with progressive loading to support training adaptations. Evaluate changes in function, not only pain sensitivity.
Vitamin D and calcium
Vitamin D and calcium support bone density and neuromuscular function when dietary intake is low. Exercise combined with adequate calcium and vitamin D may support postmenopausal bone metrics in some studies. Integrate these nutrients with weight-bearing and strength work for practical support.⁴
Menopause Joint Pain Natural Remedies
Natural remedies include daily routines with low risk and clear goals. These steps build a foundation that makes any supplement or medical plan work better. Keep the plan realistic and adjust based on your body’s feedback.
Movement and mobility habits
Aim for regular exercise that includes aerobic activity, mobility, and progressive strength training. Short sessions most days often outperform rare, long sessions. Add balance drills to reduce falls and protect function, and consider maintaining a healthy weight through consistent activity and meal planning.
Sleep and stress factors
Consistent sleep supports pain modulation and recovery. Cognitive behavioral therapy for insomnia can improve sleep quality in midlife women and may help with pain tolerance. Keep caffeine earlier in the day, and build a stable pre-sleep routine to support continuity.⁵
When lifestyle changes are not enough
If pain persists despite structured changes, ask about imaging or labs to rule out other conditions. Discuss targeted physical therapy for load management and gait or posture needs. A nutrition review can support energy balance and long-term joint health.
References
- Bai, J., Huang, W., Yan, R., & Du, X. (2025). Effects of Combined Exercise and Calcium/Vitamin D Supplementation on Bone Mineral Density in Postmenopausal Women: A Systematic Review and Meta-Analysis. Nutrients, 17(24), 3866. https://doi.org/10.3390/nu17243866
- Blumer J. Arthralgia of menopause – A retrospective review. Post Reprod Health. 2023 Jun;29(2):95-97. doi: 10.1177/20533691231172565. https://pubmed.ncbi.nlm.nih.gov/37127408/
- National Institutes of Health, Office of Dietary Supplements. (n.d.). Omega-3 fatty acids: Fact sheet for consumers. U.S. Department of Health & Human Services. https://ods.od.nih.gov/factsheets/Omega3FattyAcids-Consumer/
- National Institutes of Health, Office of Dietary Supplements. (n.d.). Vitamin D: Fact sheet for consumers. U.S. Department of Health & Human Services. https://ods.od.nih.gov/factsheets/VitaminD-Consumer/
- Ntikoudi A, Owens DA, Spyrou A, Evangelou E, Vlachou E. The Effectiveness of Cognitive Behavioral Therapy on Insomnia Severity Among Menopausal Women: A Scoping Review. Life (Basel). 2024 Oct 31;14(11):1405. doi: 10.3390/life14111405. https://pmc.ncbi.nlm.nih.gov/articles/PMC11595697/
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.